When you think about your health, the picture that probably comes to your mind is of your heart, lungs, kidneys, or brain. But did you know that your oral health plays a crucial role in your entire body’s well-being?
Most people don’t realize it, but your mouth serves more purposes than just chewing and smiling. It reflects your body’s internal health, and sometimes, it’s the first place problems show up. As dentists, we can tell many things about your general health by just looking inside your mouth.
Let’s dive into how your oral health is connected to your overall health, and why taking care of your teeth and gums is one of the best things you can do for your body.
🧬 The Mouth-Body Connection: What Is It?
Your mouth is full of bacteria, most of which are harmless. When you brush and floss daily, you keep these in balance. But if oral hygiene is neglected, harmful bacteria can grow rapidly, leading to gum inflammation (gingivitis or periodontitis) and bleeding gums.
This creates an open door for bacteria and inflammatory chemicals to enter the bloodstream and travel to other organs, including your heart, lungs, brain, and even kidneys.
This is what physicians and dentists call the oral-systemic connection — the idea that your oral health is directly linked to the health of your entire body.
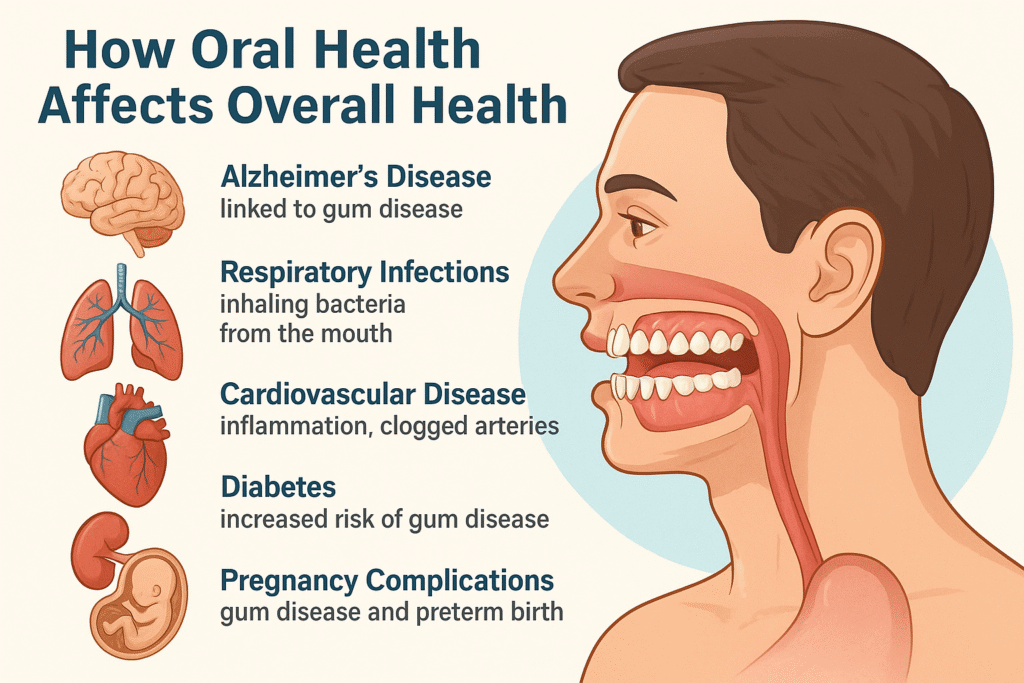
⚠️ Health Conditions Linked to Poor Oral Health
Here are some of the major ways your mouth can affect your body:
1. Cardiovascular Disease
Studies have found that people with gum disease (periodontitis) are more likely to suffer from heart problems like clogged arteries, heart attacks, and strokes. When gums are inflamed, the body produces inflammatory markers like C-reactive protein (CRP). These markers can worsen atherosclerosis, a condition where arteries become hardened and narrowed.
Bacteria from the mouth can also stick to blood vessel walls and contribute to plaque formation, raising the risk of heart attacks and strokes.
People with gum disease are up to 3 times more likely to have a heart attack.
2. Diabetes
If you have uncontrolled diabetes, the glucose level in your blood and saliva becomes high, which weakens your body’s immune system and makes it harder to fight infections, including gum infections. It will delay the healing process due to the compromised immune system.
On the flip side, if you have unhealthy gums, it will also raise the blood sugar levels, making diabetes hard to manage. Almost 25% of U.S. adults with diabetes, ages 50 and older, have severe tooth loss, compared with about 16% of those without diabetes.
3. Respiratory Infections
Your mouth is home to hundreds of species of bacteria. When you maintain good oral hygiene (by brushing, flossing, and visiting your dentist regularly), these bacteria stay in balance and don’t cause much harm. However, if you have poor oral hygiene or tooth decay, harmful bacteria from the mouth can be inhaled into the lungs, especially during sleep or while lying flat during dental treatment. This can cause:
Pneumonia
Bronchitis
Worsening of chronic lung diseases like COPD (Chronic Obstructive Pulmonary Disease)
Maintaining good oral hygiene is especially critical for hospitalized or elderly patients who are more at risk of complications.
🤰 4. Pregnancy Complications
Pregnant women with gum disease are at a higher risk of premature birth and low birth weight. That’s why dental checkups are especially important during pregnancy.
Gum disease(Gingivitis) causes bacteria and inflammatory markers to enter the bloodstream and can reach the placenta. Once this occurs, the mother is at greater risk of pregnancy complications and pre-term delivery.
Pregnant women should see a dentist early in pregnancy and maintain proper brushing and flossing habits to minimize risks.
🧠 5. Alzheimer’s and Brain Health
Chronic gum infections may allow certain bacteria (like Porphyromonas gingivalis) to travel through the bloodstream or up the nerves into the brain. This can trigger inflammation and possibly contribute to cognitive decline.
Although more research is needed, the early evidence is strong enough to emphasize gum care as a part of brain health in older adults.
⚠️ Symptoms That Your Oral Health May Be Affecting Your Body
Don’t ignore these signs — they could be early indicators of both oral and systemic health issues:
1. Bleeding gums when brushing or flossing
2. Bad breath that doesn’t go away
3. Swollen, red, or painful gums
4. Loose or shifting teeth
5. Receding gums exposing the tooth root
6. Frequent mouth infections or abscesses
If you’re seeing one or more of these symptoms, it’s time to schedule a dental visit.
Now let’s discuss some health conditions which has a direct impact on oral health;
1. Medications
Many drugs prescribed for common conditions like high blood pressure, depression, or allergies cause dry mouth (xerostomia) as a side effect. Saliva plays a crucial role in cleaning the mouth and neutralizing acids. These medicines can be antidepressants, anti-hypertensive drugs, diuretics, anti-histamines, chemotherapeutic agents, and muscle relaxants. When saliva production drops, the risk of tooth decay, gum irritation, and bad breath rises sharply. In some cases, dry mouth can also cause painful mouth sores or a burning sensation on the tongue.
2. Cancer
Those undergoing cancer treatment, particularly chemotherapy or radiation therapy to the head or neck, often deal with severe oral side effects, including damage to the salivary glands. It can result in painful sores, extreme dryness, and difficulty eating or speaking. Additionally, the immune system is weakened, increasing the likelihood of oral infections or delayed healing after dental procedures.
3. Pregnancy Complications
Hormonal changes, especially during pregnancy and menopause, can impact oral tissues. Pregnant women may experience swollen, bleeding gums, known as “pregnancy gingivitis,” due to increased blood flow and hormonal fluctuations. After menopause, estrogen levels drop, which may lead to bone loss in the jaw, dry mouth, and loosening of teeth — all of which require attention to prevent further dental complications.
Conclusion
Your systemic health and oral health are inseparable. If you have a chronic illness, take medications regularly, or are experiencing hormonal shifts, don’t overlook your mouth — it may be the first place those internal changes show.
Many people overlook dental checkups when dealing with systemic issues, but the truth is: your mouth can be the earliest warning sign of a deeper health problem. That’s why dentists play a critical role not just in maintaining your smile but in supporting your overall well-being.

